Chronic Venous Insufficiency Management: Comprehensive Care for Advanced Vein Disease
Chronic venous insufficiency represents one of the most complex and challenging conditions in venous medicine, requiring sophisticated diagnostic approaches, comprehensive treatment strategies, and ongoing management to prevent progression and optimize patient outcomes. This progressive condition affects millions of Americans and can significantly impact quality of life if not properly diagnosed and managed by experienced vein specialists who understand the intricacies of advanced venous disease.
BASS Vein Center's expertise in chronic venous insufficiency management has been developed through decades of experience treating patients with advanced venous disease, from early-stage insufficiency to complex cases involving skin changes, venous ulcers, and other serious complications. The center's comprehensive approach to chronic venous insufficiency combines advanced diagnostic capabilities, multiple treatment modalities, and long-term management strategies to provide patients with optimal outcomes and improved quality of life.
Understanding chronic venous insufficiency requires appreciating both the complex pathophysiology underlying the condition and the multifaceted approach required for effective management. This condition represents a spectrum of venous disease that can range from mild symptoms to severe complications, making individualized treatment planning and ongoing monitoring essential components of successful care.
Understanding the Pathophysiology of Chronic Venous Insufficiency
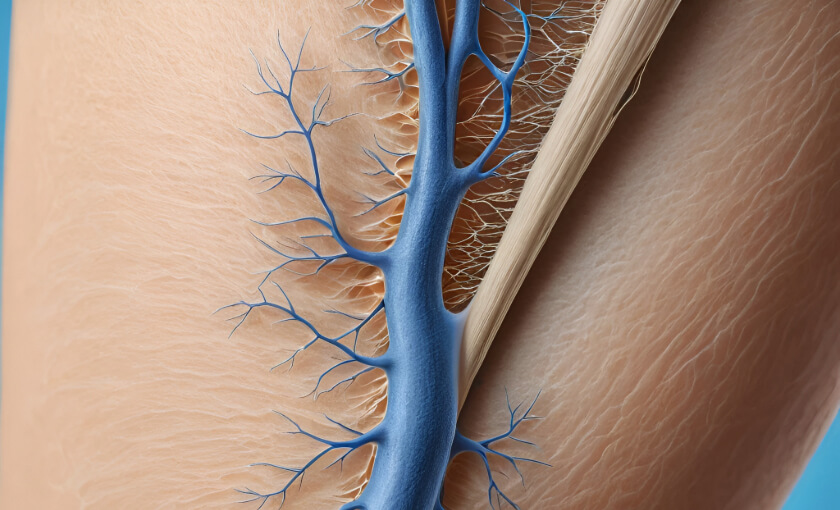
Chronic venous insufficiency develops when the venous system fails to adequately return blood from the legs to the heart, resulting in increased venous pressure, blood pooling, and a cascade of physiological changes that can lead to progressive symptoms and complications. Understanding this complex pathophysiology is essential for developing effective treatment strategies and preventing disease progression.
The venous system relies on a series of one-way valves to prevent blood from flowing backward due to gravity when standing or sitting. When these valves become damaged or incompetent, blood begins to pool in the leg veins, causing increased pressure throughout the venous system. This increased pressure, known as venous hypertension, is the fundamental problem underlying chronic venous insufficiency.
Valve incompetence can result from various factors, including genetic predisposition, previous blood clots, trauma, pregnancy, prolonged standing or sitting, and aging. Once valve function is compromised, the resulting venous hypertension creates a self-perpetuating cycle where increased pressure causes further valve damage and progressive worsening of the condition.
The effects of chronic venous hypertension extend beyond the venous system itself, affecting the surrounding tissues, skin, and lymphatic system. Increased venous pressure causes fluid to leak from the blood vessels into the surrounding tissues, leading to swelling, inflammation, and eventually tissue damage if left untreated.
Microcirculatory changes occur as chronic venous insufficiency progresses, with alterations in capillary function, tissue oxygenation, and cellular metabolism. These changes contribute to the skin changes, poor wound healing, and other complications that characterize advanced chronic venous insufficiency.
The inflammatory response triggered by chronic venous hypertension plays a crucial role in disease progression, with inflammatory mediators contributing to tissue damage, fibrosis, and the development of complications such as lipodermatosclerosis and venous ulcers.
Clinical Presentation and Staging of Chronic Venous Insufficiency
Chronic venous insufficiency presents with a wide spectrum of symptoms and signs that can range from mild discomfort to severe complications that significantly impact quality of life. Understanding this clinical spectrum is essential for accurate diagnosis, appropriate treatment planning, and monitoring of disease progression.
Early-stage chronic venous insufficiency often presents with symptoms that may be subtle or attributed to other causes, including leg heaviness, aching, fatigue, and swelling that worsens throughout the day. These symptoms are often worse after prolonged standing or sitting and may improve with leg elevation or walking.
Visible signs of chronic venous insufficiency include varicose veins, spider veins, and ankle swelling that may initially be intermittent but becomes more persistent as the condition progresses. These visible changes often prompt patients to seek medical evaluation, providing opportunities for early intervention.
Progressive symptoms develop as chronic venous insufficiency advances, including increased pain, more persistent swelling, night cramps, and restless leg syndrome. Patients may also notice that their symptoms become less responsive to simple measures like leg elevation or compression stockings.
Skin changes represent more advanced manifestations of chronic venous insufficiency and include hyperpigmentation, eczema, lipodermatosclerosis, and atrophie blanche. These changes typically occur in the lower leg and ankle area and indicate significant venous hypertension and tissue damage.
Advanced complications of chronic venous insufficiency include venous ulcers, which represent the most severe manifestation of the condition. These ulcers typically develop around the ankle area and can be difficult to heal without addressing the underlying venous insufficiency.
The CEAP classification system provides a standardized approach to staging chronic venous insufficiency based on clinical signs, etiology, anatomy, and pathophysiology. This system helps guide treatment decisions and allows for consistent communication among healthcare providers about disease severity and progression.
Comprehensive Diagnostic Evaluation
Accurate diagnosis of chronic venous insufficiency requires a comprehensive evaluation that combines clinical assessment, detailed history taking, and advanced diagnostic testing to identify the extent and severity of venous disease and guide appropriate treatment planning.
Clinical examination forms the foundation of chronic venous insufficiency diagnosis, involving detailed assessment of symptoms, visible signs of venous disease, and physical findings that may indicate underlying venous hypertension. This examination should be performed with the patient standing to allow for proper evaluation of venous filling and valve function.
Venous duplex ultrasound represents the gold standard for diagnosing chronic venous insufficiency, providing detailed information about vein anatomy, valve function, and blood flow patterns throughout the venous system. This non-invasive test can identify areas of reflux, obstruction, and other abnormalities that contribute to venous insufficiency.
Advanced imaging studies may be necessary in complex cases or when planning surgical interventions. These studies might include CT venography, MR venography, or invasive venography to provide detailed anatomical information about the deep venous system and identify any obstructions or abnormalities.
Hemodynamic testing can provide additional information about venous function and the severity of venous insufficiency. Tests such as air plethysmography, photoplethysmography, and venous pressure measurements can help quantify the degree of venous dysfunction and monitor treatment response.
Laboratory studies may be indicated to evaluate for underlying conditions that might contribute to chronic venous insufficiency or affect treatment planning. These might include coagulation studies, inflammatory markers, or tests for autoimmune conditions.
Wound assessment is crucial for patients with venous ulcers, involving detailed evaluation of wound characteristics, bacterial colonization, and healing potential. This assessment helps guide wound care strategies and monitor healing progress.
Treatment Strategies for Chronic Venous Insufficiency
Effective management of chronic venous insufficiency requires a comprehensive, individualized approach that addresses the underlying venous dysfunction while managing symptoms and preventing complications. Treatment strategies must be tailored to the severity of disease, patient factors, and individual treatment goals.
Conservative management forms the foundation of chronic venous insufficiency treatment and includes compression therapy, lifestyle modifications, and medical management of symptoms. These conservative measures are often effective for early-stage disease and serve as important adjuncts to more invasive treatments in advanced cases.
Compression therapy represents the cornerstone of conservative management, using graduated compression stockings or bandages to counteract venous hypertension and improve venous return. The appropriate level of compression must be carefully selected based on disease severity, patient tolerance, and individual circumstances.
Lifestyle modifications that can improve chronic venous insufficiency include regular exercise, weight management, leg elevation, and avoiding prolonged standing or sitting. These modifications help reduce venous pressure and improve overall venous function.
Medical management may include medications to improve venous tone, reduce inflammation, or manage specific symptoms such as pain or swelling. While medications alone are rarely curative, they can provide valuable symptom relief and support other treatment modalities.
Interventional treatments for chronic venous insufficiency include various procedures designed to eliminate venous reflux and restore normal venous function. These treatments might include endovenous ablation, sclerotherapy, or surgical procedures, depending on the specific anatomy and severity of disease.
Advanced surgical procedures may be necessary for complex cases of chronic venous insufficiency, particularly those involving deep venous obstruction or severe valve incompetence. These procedures require specialized expertise and careful patient selection to achieve optimal outcomes.
Managing Complications of Chronic Venous Insufficiency
The complications of chronic venous insufficiency require specialized management approaches that address both the underlying venous disease and the specific complications that have developed. Understanding these complications and their management is essential for preventing progression and optimizing patient outcomes.
Venous ulcers represent the most serious complication of chronic venous insufficiency and require comprehensive management that addresses both wound healing and the underlying venous dysfunction. Effective ulcer management involves appropriate wound care, compression therapy, and treatment of the underlying venous insufficiency.
Wound care for venous ulcers involves careful assessment of wound characteristics, appropriate debridement when necessary, and selection of dressing materials that promote healing while managing exudate and preventing infection. The wound care approach must be individualized based on wound characteristics and patient factors.
Infection management is crucial for venous ulcers, as bacterial colonization and infection can significantly impair healing and lead to serious complications. This may involve topical or systemic antibiotics, depending on the extent and severity of infection.
Skin changes associated with chronic venous insufficiency, such as eczema and lipodermatosclerosis, require specialized dermatological management that may include topical medications, moisturizers, and protection from further trauma or irritation.
Pain management for chronic venous insufficiency may involve various approaches, including compression therapy, elevation, medications, and treatment of the underlying venous dysfunction. Effective pain management is important for maintaining quality of life and treatment compliance.
Lymphedema management may be necessary for patients with chronic venous insufficiency who develop secondary lymphatic dysfunction. This may involve specialized compression therapy, manual lymphatic drainage, and other lymphedema management techniques.
Long-Term Management and Monitoring
Chronic venous insufficiency is a progressive condition that requires ongoing management and monitoring to prevent complications, optimize treatment outcomes, and maintain quality of life. Understanding the principles of long-term management is essential for both patients and healthcare providers.
Regular follow-up appointments are essential for monitoring disease progression, assessing treatment effectiveness, and identifying any new complications that may develop. The frequency of follow-up visits depends on disease severity and treatment complexity.
Surveillance imaging may be recommended to monitor the effectiveness of interventional treatments and identify any recurrence of venous reflux. This monitoring helps guide decisions about additional treatments and long-term management strategies.
Compression therapy compliance is crucial for long-term success in managing chronic venous insufficiency. Patients need ongoing education and support to maintain compliance with compression therapy recommendations.
Lifestyle modification reinforcement helps ensure that patients continue to follow recommendations for exercise, weight management, and other lifestyle factors that can impact venous health. Ongoing education and support are important for maintaining these beneficial changes.
Complication prevention strategies focus on identifying and addressing risk factors for disease progression and complications. This may involve regular skin assessment, wound prevention measures, and early intervention for any concerning changes.
Quality of life assessment helps monitor the impact of chronic venous insufficiency and its treatment on patient well-being. This assessment can guide treatment modifications and identify areas where additional support may be beneficial.
Multidisciplinary Approach to Complex Cases
Complex cases of chronic venous insufficiency often benefit from a multidisciplinary approach that brings together specialists from various fields to provide comprehensive care. Understanding this collaborative approach helps ensure that patients receive optimal care for all aspects of their condition.
Vascular surgery consultation may be necessary for patients with complex venous anatomy or those requiring advanced surgical procedures. Vascular surgeons bring specialized expertise in complex venous reconstructions and deep venous interventions.
Dermatology involvement is often beneficial for patients with significant skin changes or complications related to chronic venous insufficiency. Dermatologists can provide specialized care for eczema, infections, and other skin-related complications.
Wound care specialists play a crucial role in managing patients with venous ulcers, providing expertise in advanced wound care techniques, dressing selection, and healing optimization strategies.
Lymphedema therapists may be involved in the care of patients who develop secondary lymphatic dysfunction as a result of chronic venous insufficiency. These specialists provide expertise in compression therapy and lymphatic drainage techniques.
Physical therapy consultation can help patients develop appropriate exercise programs and learn techniques for improving venous circulation and overall functional capacity.
Nutritional counseling may be beneficial for patients who need to lose weight or who have nutritional deficiencies that might impair wound healing or overall health.
Patient Education and Self-Management
Effective management of chronic venous insufficiency requires active patient participation and understanding of the condition and its treatment. Comprehensive patient education is essential for achieving optimal outcomes and preventing complications.
Disease education helps patients understand the nature of chronic venous insufficiency, its progression, and the importance of ongoing treatment and monitoring. This understanding promotes better compliance with treatment recommendations and earlier recognition of complications.
Compression therapy education includes proper fitting, application, and care of compression garments. Patients need to understand the importance of consistent use and proper technique to achieve optimal benefits from compression therapy.
Skin care education focuses on proper hygiene, moisturizing, and protection of the legs and feet. Patients need to understand how to inspect their skin for changes and when to seek medical attention for concerning findings.
Activity and exercise guidance helps patients understand appropriate activities that can improve venous circulation while avoiding activities that might worsen their condition. This education should be individualized based on patient capabilities and preferences.
Warning sign recognition teaches patients to identify symptoms or changes that might indicate disease progression or complications requiring medical attention. Early recognition and treatment of complications can prevent more serious problems.
Self-monitoring techniques help patients track their symptoms, compliance with treatment, and overall condition. This self-monitoring can help identify trends and guide treatment modifications.
Cost-Effectiveness and Healthcare Economics
Understanding the economic aspects of chronic venous insufficiency management is important for both patients and healthcare systems, as this condition represents a significant healthcare burden that can be reduced through effective management.
Healthcare costs associated with chronic venous insufficiency are substantial, particularly when complications such as venous ulcers develop. Early intervention and effective management can significantly reduce these costs by preventing complications and reducing the need for extensive wound care.
Cost-effectiveness of different treatment approaches varies depending on disease severity, patient factors, and treatment goals. Comprehensive evaluation of cost-effectiveness should consider both direct medical costs and indirect costs such as lost productivity and reduced quality of life.
Insurance coverage for chronic venous insufficiency treatment is generally good when the condition is properly documented and treatment is deemed medically necessary. Understanding insurance requirements and documentation needs helps ensure appropriate coverage for necessary treatments.
Prevention strategies that focus on early intervention and lifestyle modifications can provide excellent cost-effectiveness by preventing disease progression and complications. These strategies represent important opportunities for reducing the overall healthcare burden of chronic venous insufficiency.
Quality metrics for chronic venous insufficiency management help assess the effectiveness of different treatment approaches and identify opportunities for improvement in care delivery and outcomes.
Future Directions in Chronic Venous Insufficiency Management
The field of chronic venous insufficiency management continues to evolve with advances in diagnostic techniques, treatment modalities, and understanding of disease pathophysiology that promise to improve outcomes for patients with this challenging condition.
Biomarker development may provide new tools for diagnosing chronic venous insufficiency, monitoring disease progression, and predicting treatment outcomes. These biomarkers could help guide treatment decisions and improve patient selection for different interventions.
Advanced imaging techniques continue to improve, providing better visualization of venous anatomy and function. These advances may help identify disease earlier and guide more precise treatment approaches.
Novel treatment modalities under development include new devices, medications, and biological therapies that may provide additional options for patients with chronic venous insufficiency. These developments could expand treatment options and improve outcomes for challenging cases.
Regenerative medicine approaches, including stem cell therapy and tissue engineering, may provide new options for treating complications such as venous ulcers and promoting healing in patients with advanced disease.
Telemedicine and remote monitoring technologies may improve access to specialized care and enable better monitoring of patients with chronic venous insufficiency, particularly those in underserved areas or with mobility limitations.
Conclusion: Excellence in Complex Venous Disease Management
Chronic venous insufficiency represents one of the most challenging conditions in venous medicine, requiring comprehensive expertise, advanced diagnostic capabilities, and individualized treatment approaches to achieve optimal outcomes. The complexity of this condition demands specialized knowledge and experience that goes beyond basic vein treatment to encompass the full spectrum of advanced venous disease management.
The progressive nature of chronic venous insufficiency makes early recognition and intervention crucial for preventing complications and maintaining quality of life. Effective management requires a comprehensive approach that addresses not only the underlying venous dysfunction but also the various complications and quality of life issues that can arise from this condition.
BASS Vein Center's expertise in chronic venous insufficiency management, developed through decades of experience with complex venous disease, provides patients with access to the comprehensive care needed to effectively manage this challenging condition. The center's multidisciplinary approach and commitment to ongoing education ensure that patients receive the most current and effective treatments available.
For individuals dealing with the complex challenges of chronic venous insufficiency, having access to specialized expertise and comprehensive management strategies can make the difference between progressive disability and maintained quality of life. The combination of advanced diagnostic capabilities, multiple treatment modalities, and ongoing management support provides the foundation for optimal outcomes in this challenging condition.
Don't let chronic venous insufficiency continue to progress and impact your quality of life when comprehensive management strategies can help control the condition and prevent complications. Contact BASS Vein Center today at (925) 489-1684 to learn more about comprehensive chronic venous insufficiency management and discover how specialized expertise can help you achieve better outcomes and improved quality of life. Your journey toward better management of this complex condition begins with a consultation with specialists who have the knowledge and experience to provide the comprehensive care you need.
Note: Coverage varies between insurance plans. Please check with your insurance provider before scheduling. BASS Vein Center will verify your benefits so you understand any out-of-pocket costs ahead of treatment.
Medical Disclaimer: The information provided in this blog is for educational and informational purposes only and is not intended as medical advice, diagnosis, or treatment. BASS Medical Group does not endorse any specific tests, treatments, procedures, or opinions referenced in this content. Individual results may vary. Always consult with your physician or a qualified healthcare provider regarding any medical concerns or before making changes to your health regimen.




