Varicose Vein Treatment Guide
Understanding causes, symptoms, diagnosis, and treatment options

Varicose veins are enlarged, twisted surface veins that most commonly develop in the legs. They occur when vein valves weaken and allow blood to pool instead of flowing efficiently back to the heart.
For some people, varicose veins are primarily cosmetic. For others, they may cause discomfort, heaviness, swelling, or skin changes. This guide explains how varicose veins develop, how they are evaluated, and what treatment options may be available.
What Causes Varicose Veins?
Varicose veins develop when the valves inside leg veins do not close properly. This condition, called venous reflux, increases pressure within the vein and causes it to enlarge.
Several factors are associated with increased risk:

Age
As you get older, the valves in your veins may weaken, making it harder for blood to flow properly.

Gender
Women are more likely to develop varicose veins than men, partly due to hormonal changes during pregnancy, menstruation, and menopause.

Genetics
If you have a family history of varicose veins, you may be more likely to develop them yourself.

Obesity
Being overweight or obese can put extra pressure on your veins, making it more difficult for blood to circulate properly.

Prolonged standing or sitting
Jobs that require long periods of standing or sitting can lead to weakened valves in the veins.

Pregnancy
Pregnant women experience increased pressure on their veins due to the growing fetus and hormonal changes, which can lead to varicose veins.

Injury
Injury or trauma to the legs may damage the veins and lead to varicose veins over time.
Other medical conditions: Some medical conditions, such as deep vein thrombosis (DVT)or chronic venous insufficiency (CVI), may increase the risk of developing varicose veins.
Not everyone with risk factors develops varicose veins, but symptoms should be evaluated if they persist.
How Are Varicose Veins Diagnosed?

Diagnosis begins with a medical history and physical examination.
A duplex ultrasound is typically used to:
- Evaluate blood flow
- Identify venous reflux
- Detect underlying vein dysfunction
Ultrasound findings help determine whether conservative management or procedural treatment is appropriate.
Advanced imaging (such as venography or MRI-based studies) is rarely required for routine varicose vein evaluation.
Conservative (Non-Procedural) Management
Non-invasive approaches for treating varicose veins are usually the first line of treatment, particularly for mild to moderate cases. These approaches aim to improve blood flow in the affected veins, reduce swelling, and relieve symptoms such as pain and discomfort.
Here are some non-invasive approaches for treating varicose veins:
Compression Therapy
Medical-grade compression stockings support circulation and may reduce swelling and discomfort.
Activity & Movement
Regular walking and leg elevation can help support venous return.
Weight Management
Reducing excess pressure on the legs may improve symptoms.
Non-invasive approaches for treating varicose veins may provide relief from symptoms and prevent the condition from worsening. However, they may not be effective for severe cases, and more invasive treatments may be required. If you are experiencing symptoms of varicose veins, it's important to seek medical attention for proper diagnosis and treatment.
Minimally Invasive Treatment Options
When ultrasound confirms venous reflux, in-office procedures may be recommended. Treatment selection depends on vein anatomy, symptom severity, and overall health. Your physician will review imaging findings and discuss appropriate options.

Sclerotherapy
Sclerotherapy involves injecting a solution directly into smaller varicose or spider veins. The solution irritates the vein lining, causing it to collapse and gradually be reabsorbed by the body. It is commonly used for cosmetic veins and smaller symptomatic vessels.

Endovenous laser treatment (EVLT)
EVLT uses a thin catheter to deliver laser energy inside a refluxing vein. The heat causes the vein to close, redirecting blood flow to healthier veins. The procedure is performed under local anesthesia in an outpatient setting.

Radiofrequency Ablation (RFA)
RFA uses controlled radiofrequency energy to treat larger refluxing veins. A catheter is placed inside the vein, and thermal energy is applied to seal it closed. Blood flow is then naturally redirected to functioning veins.

VenaSeal™
VenaSeal uses a medical adhesive delivered through a catheter to close the affected vein. Because it does not rely on thermal energy, it may be appropriate for certain patients based on anatomy and clinical evaluation. Your physician will determine whether this option is suitable.
Ambulatory Phlebectomy
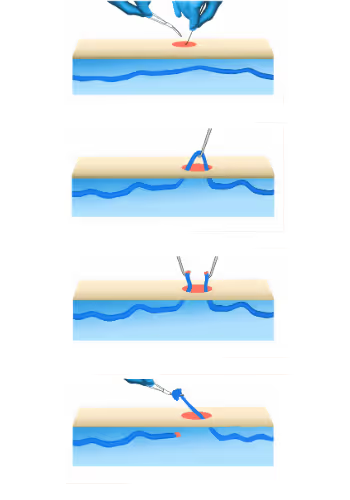
Ambulatory phlebectomy removes larger surface varicose veins through very small skin openings. The procedure is typically performed under local anesthesia. It may be recommended when veins are too large for injection therapy alone.
Minimally invasive treatments for varicose veins are a popular option for those who have not found relief from non-invasive treatments or prefer less invasive options. These treatments use advanced medical technology to target the affected veins and close them off, redirecting blood flow to healthier veins. Here are some minimally invasive treatments for varicose veins:
Are Surgical Procedures Ever Needed?
Traditional vein stripping or ligation is uncommon today and typically reserved for complex or advanced cases when minimally invasive options are not appropriate. Your physician will determine whether surgical treatment is necessary based on imaging and symptoms.
Recovery After Vein Treatment
%20(1).jpg)
Recovery varies depending on the procedure performed.Many minimally invasive treatments allow patients to return to normal activity relatively quickly, although temporary bruising, mild soreness, or swelling may occur. Your physician will provide individualized instructions regarding:
- Compression use
- Activity level
- Follow-up visits
Long-term vein health may involve continued lifestyle adjustments and monitoring.
Who Treats Varicose Veins?
.jpeg)
Varicose veins are commonly treated by physicians with specialized training in vascular or venous disease. At BASS Vein Center, board-certified vascular surgeons provide evaluation and treatment across multiple East Bay locations. Care plans are based on ultrasound findings and individual patient needs.
When Should You Seek Evalution By a Vein Specialist?
You may consider scheduling an evaluation if you experience:
- Compression use
- Activity level
- Follow-up visits
Early evaluation can help determine whether symptoms are related to venous reflux or another condition.
Frequently Asked Questions
The best treatment depends on ultrasound findings, vein anatomy, and symptom severity. Minimally invasive procedures are commonly used when reflux is confirmed.
Visible varicose veins typically do not resolve without treatment. Symptoms may fluctuate over time.
Compression stockings may help manage symptoms but do not repair dysfunctional vein valves.
Coverage often depends on documented symptoms and ultrasound findings. Cosmetic treatment of spider veins may not be covered.
